 The most successful businesses are the ones that keep clients in the loop. For medical practitioners, your communications platform (phone, email, and notification systems) is your foundation to the management of your patient population and success of your business operations. Consumer-driven healthcare is the new reality, and medical practices rely now more than ever on patient satisfaction and experience to maintain a profitable practice and to sustain reimbursements.
The most successful businesses are the ones that keep clients in the loop. For medical practitioners, your communications platform (phone, email, and notification systems) is your foundation to the management of your patient population and success of your business operations. Consumer-driven healthcare is the new reality, and medical practices rely now more than ever on patient satisfaction and experience to maintain a profitable practice and to sustain reimbursements.
And what many fail to realize is that the large hospital-owned groups are investing in advanced communications systems designed to make that growth easier.
The point of all of this is to say that if your system is too outdated; your patients may choose to find a practice that provides them with a better user-experience around scheduling, notifications and general communication with their provider.
Rather than rely on older analog phone systems and outdated contact center software, your medical office can turn to IP Telephony solutions with Unified Communications features to help manage your daily patient matrix management and care.
Why IP Telephony?
Modern phone system technology delivers so much more today than just a dial tone. Phone systems are constantly changing, and are growing to be part of converged networks that seamlessly tie voice with other Unified Communications (UC) features like data, video conferencing, instant messaging, single-number reach, appointment scheduling, and other business-critical communications tools and applications.
Voice over Internet Protocol (VoIP) is a technology that allows telephone calls to be made over computer networks. And while it’s not a new technology, many organizations have not yet transitioned from older technologies to IP telephony (IPT) solutions. IPT converts analog voice signals into digital data packets and supports real-time, two-way transmission of conversations using the internet. So rather than needing to install and pay for multiple lines in your office building, you can tie your phones directly into your internet network rather than needing to utilize a Plain Old Telephone Service (POTS) phone.
Here are some of the ways that Medical Professionals can benefit from IPT systems:
Increased Cost-Effectiveness
Operating IPT systems can be less expensive than traditional wired telephone systems because they require less hardware, less maintenance, and have lower OPEX costs than POTS systems.
Not all IPT systems are created equally though. When you look at the total cost of ownership for IPT systems, you’ll find that the best systems lower capital, implementation, and operational costs than standard POTS systems.
Plus, maintenance of your telephony system should be easier with all of your organization's voice and data traffic integrated into one physical network. Although there is an initial setup cost, significant net savings can result from managing one network and not sustaining a legacy telephony system in an increasingly digital and data-centered world.
Enhanced Quality
For medical practices, much of your daily communication will always rely on person-to-person conversations. IP telephony systems provide clear voice quality so that communication with patients is never compromised. Additionally, it complements the other initiatives and investments in your practice such as Electronic Health Records.
Improved Extensibility and Accessibility
The communications industry moves at a rapid pace. The best IP telephone hardware is modular, and much of its advanced functionality is software based. This makes it easier to manage the total system. With the hardware, you can just replace or upgrade certain pieces as needed. The software can be updated to include new components and capabilities when they become available. Additionally, such advanced technologies were previously only available to large enterprise organizations with deep pockets. Today, these systems are available for small business and independent medical practices.
Advanced Applications
Many IP telephony systems can be bought in conjunction with or are already a part of, Unified Communications systems. UC offers advanced capabilities—such as appointment confirmation, emergency notification, and enterprise-level mobility—that improve the efficiency of your office’s operations.
These additional applications can modernize your communications strategies. Medical practices are operated by appointment schedules. So any gaps or lost appointments that occur during the day result in lost revenue. At the same time, managing multiple clients and appointments can be tedious, time consuming, and expensive when done manually. It may also counter your Electronic Health Record strategy. So a VoIP and UC enabled solution makes sense for independent physician practices.
Why? UC can provide you with an appointment reminder system that supports outbound reminder/service calls. This sort of application can be programmed to remind your patient populations about everything from upcoming appointments, to what the vaccination requirements are for local schools.
With the extensibility that UC provides, any member of the medical office staff can keep patients aware of whatever it is they need to know. The bonus is that you benefit from increased efficiency and revenues, reduce missed appointments and last-minute cancellations, and increase customer and employee satisfaction and retention with one program.
Better Integration
Since many UC capabilities are software based, integration with other business systems is relatively easy. This gives your staff the ability to see who is calling your office before they pick up the phone, and gives them the opportunity to pull the patient’s profile before answering the call. The result is a patient who is favorably impressed by your company’s expert customer service and communications skills.
Whether it eases employee frustration or keeps your schedule full of confirmed appointments, we’re sure that a unified communications system with IP telephony can bring your medical practice enterprise-level communications features and mobility solutions that will modernize and benefit your organization.
To learn more about how we can help your medical practice improve patient communication and provide cost-effective business process improvements, click below to talk to one of our healthcare technology experts.


 The constant ringing of multiple alarms and
The constant ringing of multiple alarms and 
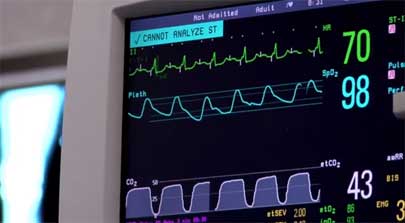
 Overhead pages, telephones ringing, and ongoing conversations between caregivers can be a source of discomfort for patients, and, as noted by The
Overhead pages, telephones ringing, and ongoing conversations between caregivers can be a source of discomfort for patients, and, as noted by The  The healthcare industry has traditionally been dependent on data communication methods through computer-based information systems. Recent studies, however, have shown that clinicians no longer wish to be confined to a PC to retrieve critical information such as lab results, STAT orders, radiology reports and other
The healthcare industry has traditionally been dependent on data communication methods through computer-based information systems. Recent studies, however, have shown that clinicians no longer wish to be confined to a PC to retrieve critical information such as lab results, STAT orders, radiology reports and other 
 Today’s healthcare professionals are highly mobile and as a result require tools that provide instant access to crucial information and communications with their colleagues. Safety, quality, costs and staffing shortages are just some of the critical factors impacting patient care in hospitals today, making efficient communications more essential than ever before. According to the
Today’s healthcare professionals are highly mobile and as a result require tools that provide instant access to crucial information and communications with their colleagues. Safety, quality, costs and staffing shortages are just some of the critical factors impacting patient care in hospitals today, making efficient communications more essential than ever before. According to the 
 What do you do when you need to deliver time-sensitive information to hundreds, or even thousands of people? Do you have a mass notification system in place to help get the word out quickly and efficiently? There are times when alerts sent to the general population of a hospital, school or business are not only helpful, but necessary.
What do you do when you need to deliver time-sensitive information to hundreds, or even thousands of people? Do you have a mass notification system in place to help get the word out quickly and efficiently? There are times when alerts sent to the general population of a hospital, school or business are not only helpful, but necessary. 