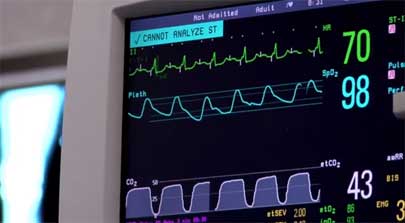
 The constant ringing of multiple alarms and notifications from devices continues to contribute to the phenomenon called “alarm fatigue” that is putting hospital patients nationwide at serious risk.
The constant ringing of multiple alarms and notifications from devices continues to contribute to the phenomenon called “alarm fatigue” that is putting hospital patients nationwide at serious risk.
Alarm fatigue occurs when doctors, residents, nurses, and staff become de-sensitized to emergency alarms and subconsciously shut them out. With some hospitals experiencing nearly 12,000 alarms -a- day, on average, it’s easy to understand why alarm fatigue happens and is dangerous.
For the last three years, alarm fatigue has ranked at the top of health and IT hazards list. The issue is so critical; in fact, that the Joint Commission, the leading independent performance standards certifier for healthcare facilities in the United States, issued a new National Patient Safety Goal (NPSG) this January, which requires accredited hospitals and critical access hospitals to improve their systems.
Alarms, if improperly managed, can do more harm than good for patients. If bad information—or in this case overwhelming information—comes in, then bad decisions will go out. The more data, alarms, and technology you have—the more likely you are to make simple errors. And in hospitals, those errors are proving to be fatal.
The NPSG Requirements
The requirements addressed in this NPSG became effective as of January 1, 2014 for hospitals and critical access hospitals. As noted in the elements of performance listed in the report, the NPSG will be implemented in two phases. The first phase is heightening awareness of the potential risks associated with clinical alarms, and the second phase will introduce requirements to mitigate those risks.
This NPSG addresses clinical alarms that can compromise patient safety if they are not properly managed. This includes alarms from equipment such as cardiac monitors, IV machines, ventilators, etc. that have visual and/or auditory components (in general this NPSG will not apply to items such as nurse call systems, alerts from computerized provider order entry (CPOE), or other information technology (IT) systems).
The NPSG states:
- As of July 1, 2014, leaders establish alarm system safety as a hospital priority.
- During 2014, identify the most important alarm signals to manage based on the following: input from medical staff, clinical departments, and risk to patients.
- As of January 1, 2016, leaders establish policies and procedures for managing the alarms identified above. The following should be addressed:
- Clinically appropriate settings for alarm signals
- When alarm signals can be disabled
- When alarm parameters can be changed
- Who in the organization has the authority to set, change, or turn-off alarm parameters
- Monitoring and responding to alarm signals
- Checking individual alarm signals for accurate settings, proper operation, and detectability
- As of January 1, 2016, educate staff and licensed independent practitioners about the purpose and proper operation of alarm systems for which they are responsible.
Additional Resources
Alarm fatigue isn’t the only critical tech related issue that today’s healthcare professionals have to deal with. Mobility is constantly an issue for physicians and nurses that need to move between rooms, floors, and even buildings. Communications in particular can be a struggle for administrators trying to determine how to keep patients happy and equip staff to do their jobs—particularly when disparate systems don’t “talk” with each other.
Improving communications can actually help solve many of the other critical tech issues that hospitals are facing. How? By using utilizing a clinical workflow solution.
A clinical workflow solution can help hospital administrators mitigate the risk associated with alarm fatigue. The solution essentially cuts the noise from all communications sources down, and ties them together in a logical way. It unites all clinical information systems within hospitals into one manageable program allowing for instant access to data, helping to reduce alarm fatigue while continuing to satisfy the regulatory compliance required when running disparate systems.
The unification of the communications sources enables care providers to more effectively manage their time and resources as they serve several patients simultaneously.
You’ll know you have found a good workflow management system when its base features include:
- Lab Result Notifications
- Nurse Call Integration
- Report Availability Notifications
- Device Messaging
In addition to intelligent alerting, workflow management systems should instantly connect healthcare professionals to each other and to their patients. These systems are designed to reduce overhead noise to help create a more healing environment, and to facilitate a happier healthier patient.
Best of Breed Healthcare IT Solutions
NEC is a leading innovator and provider of healthcare technology services, with more than 50 years of experience creating cutting edge technology solutions.
Download our brochure on NEC’s Clinical Workflow Solutions from EXTENSION, INC., today, and learn more about how we can empower your organization by providing enhanced communication tools that instantly connect your employees and patients along the care continuum.


